By: Shabria L. Mayne, MS, LPC, LCMHC, NCC, DBH Candidate at Cummings Graduate Institute for Behavioral Heath Studies, written for the course DBH 9033: Emerging Trends in Integrated Care
Comorbid Disorders Among Women: The Impacts of Trauma on Women’s Health and Applied Treatment Strategies using the Biodyne Model
Abstract
The relationship between physical and mental health is explained by direct and indirect effects of past mental and physical health (Ohrnberger et al., 2017, p.43). The prevalence of traumatic experiences throughout developmental years has a significant impact on the manifestation of future comorbid conditions, particularly among women. Exposure to trauma progresses into biological changes and stress responses. For instance, various studies indicate women to have an increased prevalence of mental health diagnosis such as post-traumatic stress disorder (PTSD) and other internalizing disorders like depression and anxiety. Correspondingly, this correlates to higher rates of diagnosed medical conditions such as high blood pressure/hypertension, thyroid diseases, cardiovascular diseases (CVD), and substance abuse related disorders. A practical therapeutic encounter will be examined for the purpose of exploring this notion. Additionally, examples of effective, ongoing treatment planning employed using the Biodyne Model within integrated healthcare will be provided.
Purpose/Objectives
After reading the research presented along with the applicable case scenario, readers will be able to:
- Identify criteria for diagnosing post-traumatic stress disorder (PTSD) among women presenting with considerable symptoms of stress, anxiety, or depression.
- Compare the relationship between extensive experiences with childhood trauma and the development of adverse adult functioning.
- Recognize the connection between comorbid medical diagnosis and trauma-specific mental health diagnosis.
- Evaluate the best treatment plan to address this comorbid concern based on the Biodyne Model within integrated care delivery.
Target Audience:
Applicable to all medical and behavioral health practitioners working in various healthcare settings with advanced (applied theory) level of experience.
Findings:
There is a proven correlation between a person’s medical health and mental health. Further, the prevalence of diagnosed comorbid conditions is high among women (Mayne, 2024). A study by Davis et al. (2022) concluded that the economic burden of treating PTSD is in the billions of dollars and a high percentage of this treatment is with civilian women. The use of integrated healthcare not only treats patients therapeutically and medically, but also addresses the social determinants of health in measuring cost-effective treatment outcomes.
Key words: Trauma; Childhood trauma; Post-traumatic stress disorder; Women’s healthcare; Women’s stress; Women’s mental health; Cardiovascular disease; Integrated healthcare; Comorbid disorders; Biodyne Model
Introduction

Many patients seeking treatment in medical and behavioral health settings have preexisting histories of trauma but are often unaware of the connection between their trauma history and presenting concerns. The American Psychological Association (APA) defines trauma as an emotional response to an extreme or distressing event, usually placing one at risk for serious harm or death, which results in a lasting emotional response (American Psychological Association, 2021). Long-term reactions to traumatic experiences may include unstable emotions, anxiety-provoked flashbacks, strained relationships, sleep disturbances, and physical symptoms. As it relates to gender, women have a 2-3x higher risk of developing post-traumatic stress disorder (PTSD) compared to men (Olff, 2017). There are many research studies aimed to consider the high prevalence of comorbid health-related conditions among women. This linkage assumes that there is a significant association between mental health and physical health. For instance, Ohrnberger et al. (2017) found that present physical and mental health are explained by direct and indirect effects of past mental and physical health (p.43). Therefore, women diagnosed with a pre-existing trauma-related mental health disorder may also suffer from medically related health concerns such as cardiovascular disease (CVD).
Cardiovascular Disease
The American Heart Association (2017) identifies cardiovascular diseases (CVDs) as a group of disorders of the heart and blood vessels. To elaborate, blood flow to different areas of the body may be reduced. This reduction can be caused by a build-up of fatty deposits inside the arteries or due to blood clots. There are diverse types of cardiovascular disease, such as coronary heart disease, valve disease, peripheral artery disease, heart failure, and stroke. “There are various physical symptoms of cardiovascular disease, including chest pain, or noticeable changes in heartbeat, dizziness, or lightheadedness, swelling of the extremities (legs, ankles, or feet), and uncommon skin rashes” (Mayne, 2023). Additionally, the CDC identifies risk factors for cardiovascular disease to include high blood pressure, tobacco use, obesity, stress, diabetes, and genetics related to family history (CDC, 2023). The Centers for Disease Control and Prevention states that heart disease is the leading cause of death for women in the America (2023).
Thyroid Disease
Thyroid disease is a diagnosed medical condition in which the thyroid does not produce the appropriate number of hormones. According to the American Thyroid Association (n.d.), thyroid disease is a common occurrence among Americans, and the disease impacts more women than men with women being 5-8x more likely to have thyroid problems (2016). There are two prominent types of thyroid disease; hyperthyroidism (overactive thyroid) and hypothyroidism (underactive thyroid), both of which may be caused by preexisting conditions or may be genetic in nature. Hyperthyroidism and anxiety are interrelated due to its symptoms, and patients with hyperthyroidism may experience heightened anxiety. For instance, while current research does not support the claim that hyperthyroidism is caused by anxiety, hyperthyroidism can significantly increase stress hormone levels in patients and exacerbate PTSD symptoms such as increased heart rate, hyperactivity, and agitation (Mayne, 2023).
Trauma
Trauma Defined
While trauma is intricately linked to acts of violence, it is unique to the individual experiencing the event. Varying traumatic experiences may account for instances related to abuse (physical, sexual, and emotional), bullying, loss of a loved one or a significant breakup, child neglect, poverty, racism, accidents, and medical interventions. Exposure to traumatic experiences can have immediate and lasting effects on one’s mental health. For instance, exposure to trauma progresses into biological changes and stress responses. This includes a “complex interchange of nervous, endocrine, and immune mechanisms that involves activation of the sympathetic-adreno-medullar (SAM) axis, the hypothalamus-pituitary-adrenal (HPA) axis, and immune system” (Chu et al., 2022). Further, people impacted by trauma may develop maladaptive behaviors, to cope with this stress response, directly contributing to mental health disorders like anxiety and depression, cognitive impairment, and chronic heart disease. Table 1 defines distinct types of traumas experienced and their unique estimated prevalence.
Table 1 Interpersonal Trauma Definitions and Data Points
|
Trauma Type |
Definition |
Prevalence |
Source |
|
Child neglect & physical abuse |
When a parent or caregiver acts, or fails to act, in a way that results in physical injury to a child or adolescent, even if unintentional |
>600,000 children were victims of abuse and neglect in 2021. 76% of children are neglected, & 16% are physically abused. |
National Children’s Alliance, 2023 |
|
Sexual Assault |
Sexual violence refers to any sexual activity in which consent is not obtained or freely given |
>50% women & 1 in 3 men have experienced sexual violence. > 4 in 5 female rape survivors reported the occurrence before age 25. |
Centers for Disease Control and Prevention, 2022 |
|
Intimate partner violence |
Physical violence, sexual violence, stalking, and psychological aggression by a current or former intimate partner |
1 in 4 women & 1 in 9 men experience severe intimate partner physical violence. Women ages18-24 are most abused by an intimate partner. |
National Coalition Against Domestic Violence, 2021 |
|
Child sexual abuse |
An interaction between a child and an adult or child in which the child is used by the perpetrator for sexual stimulation. |
10% of children are sexually abused, and 0.2% are sex trafficked. |
National Children’s Alliance, 2023 |
|
Community Violence |
Exposure to intentional acts of interpersonal |
1 in 5 high school students reported being bullied on |
Federal Data Youth.gov, 2019 |
Content adopted from Gerber, M. R., & Gerber, E. B. (2019). An Introduction to Trauma and Health. Trauma-Informed Healthcare Approaches, 3–23. https://doi.org/10.1007/978-3-030-04342-1_1
Epidemiology
More than half of all women will be exposed to at least one traumatic event in their lifetime, according to the National Center for PTSD (Novotney, 2023). As stated earlier, the body’s stress response due to exposure to traumatic incidents can have adverse physiological effects. For example, the hypothalamic-pituitary-adrenal (HPA) axis controls the body’s stress response. According to Sheng et al., (2021) critical developmental stages must be attained to warrant proper functionality of the HPA axis and appropriate behavioral and physiological stress-responses in adulthood. A physical or emotional stressor may trigger an HPA axis response and because the thyroid is so associated with the HPA axis, any dysfunction in that axis will impact thyroid functioning. Furthermore, stress may increase inflammation in the body causing an increase in heart rate and blood pressure. The “fight or flight” response is explained by Chu et al., (2022) as “increased blood flow and pressure to active muscles and decreased blood flow to organs not required for rapid motor activity, increased rate of blood coagulation, cellular metabolism, muscle strength, mental activity, blood glucose concentration, and glycolysis in the liver.”
Post-Traumatic Stress Disorder
One of the most known stressor-related mental health disorders is post-traumatic stress disorder (PTSD). PTSD is a mental health disorder that some individuals may develop after experiencing a traumatic event. Symptoms are emotional, cognitive, and behavioral in nature and childhood trauma increases the severity and likelihood of developing the diagnosis. Figure 1 displays a simplistic version of the DSM-5 diagnostic criteria for posttraumatic stress disorder.
Figure 1
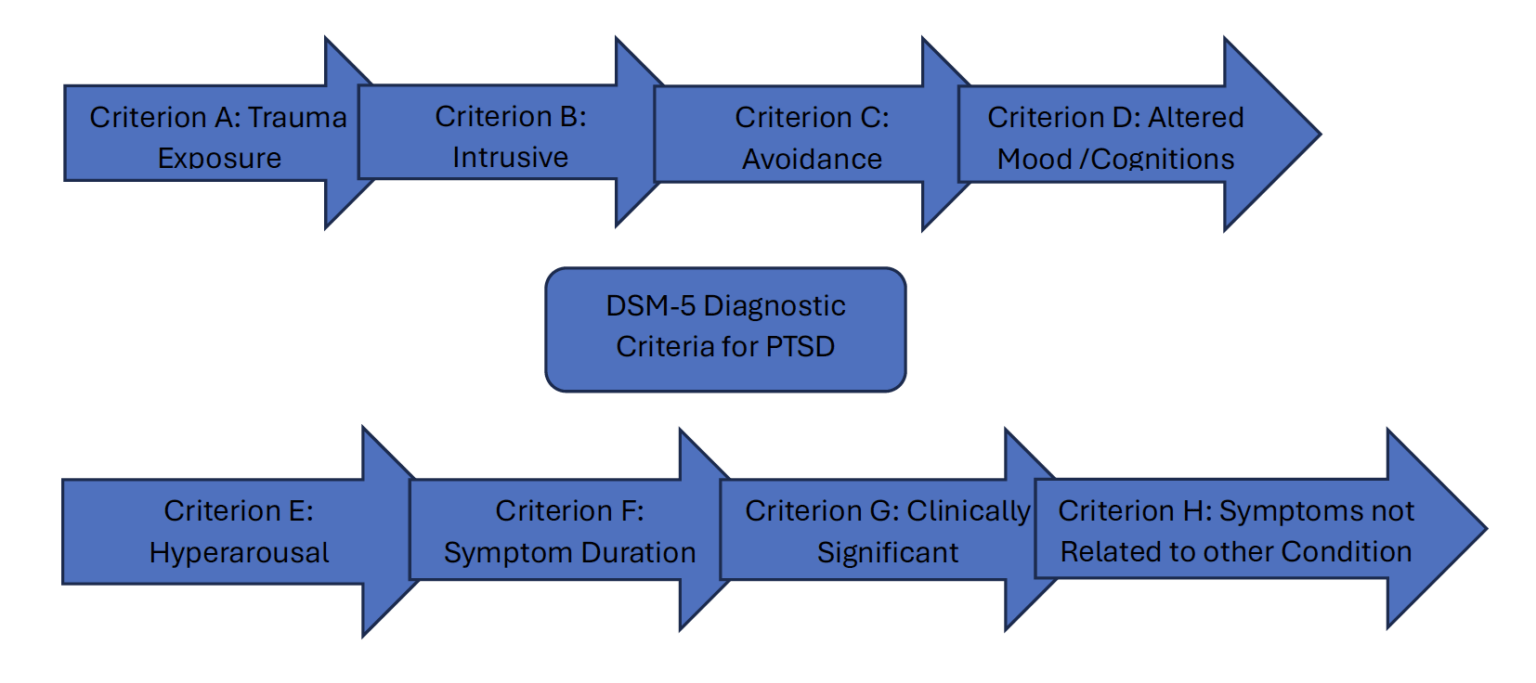 Women are at greater risk for developing PTSD and experience symptoms longer than men due to a higher exposure to interpersonal and high-impact trauma like sexual abuse. Further, it takes women 4 years to be diagnosed and obtain appropriate treatment (Companies, 2023). Repeated traumatic experiences during critical developmental years are associated with poorer early childhood brain development.
Women are at greater risk for developing PTSD and experience symptoms longer than men due to a higher exposure to interpersonal and high-impact trauma like sexual abuse. Further, it takes women 4 years to be diagnosed and obtain appropriate treatment (Companies, 2023). Repeated traumatic experiences during critical developmental years are associated with poorer early childhood brain development.
Galli et al. (2021) sought to research the role of trauma in the development of cardiovascular diseases. The authors considered various studies focusing on childhood adversities, such as family conflict and neglect, and how psychological factors created a 50% higher risk of developing CVD (2021). Overall, the authors confirmed that childhood trauma has a greater impact on adult cardiovascular health, and that the burden is worse in women due to the types of traumas experienced (p.10). Furthermore, women experience more distress than men on almost all symptoms identified on The Traumatic Experience Checklist (TEC). Women are also more likely to experience internalizing disorders like anxiety and depression (Cherry, K. 2021).
Box 1: Case Scenario
|
Case Study Janet, 44, is a single mother of two children with an extensive history of complex trauma beginning in childhood. Traumatic experiences include rearing by a parental figure with an alcohol addiction and instances of sexual abuse at the hands of her older sister. Janet reported multiple suicide attempts throughout her adolescence leading to numerous psychiatric hospitalizations. She was diagnosed with bipolar disorder at age 14, has a preexisting diagnosis of PTSD, ADHD, and a comorbid medical diagnosis of hyperthyroidism. Relationally, Janet reported various physically and verbally abusive relationships with men throughout her adulthood. Further, she reported present frequent discord with her mother (abuses alcohol), stress in managing her relationship with her partner (who is in SA recovery), and a healthy dynamic with her sister. Functionally, Janet reports she experiences mood swings ranging from significant bouts of depression to borderline mania. She routinely meets with a psychiatrist for medication management, and is prescribed the following medications: Lamotrigine, Seroquel, Abilify, Prozac, Vyvanse, and Adderall. However, she expressed interest in reducing or eliminating some of her prescribed medications. Janet reported that she smokes marijuana 2-3x weekly to manage stress. She attends Al-ANON meetings regularly to develop a support system and learn about substance abuse. Additionally, Janet engages in healthier stress-management activities such as weekly horseback riding and writing poetry. Some valuable points of consideration when developing a treatment plan for this patient include the following:
|
Trauma-Informed Care and the Biodyne Model
Trauma-Informed treatment is a therapeutic approach which primarily focuses on the belief that trauma can significantly impact an individual’s well-being, including one’s physical and mental health. A trauma-informed approach highlights three primary elements: (1) understanding trauma prevalence (2) understanding how trauma affects all individuals involved and (3) responding by putting such knowledge into practice (SAMHSA, 2012, p.4). The benefits of trauma-informed care are that it employs an integrated healthcare approach during treatment to arrive at specified goals responding to comorbid conditions. Figure 2 highlights the guiding principles of trauma-informed care employed within the integrated healthcare system.
Figure 2: Trauma-Informed Care
 Treatments such as cognitive behavioral therapy (CBT) and prolonged exposure therapy are proven effective in treating patients diagnosed with PTSD. Comparable to principles of the Biodyne Model, trauma-informed care allows patients to be fully engaged in their treatment process through interdisciplinary collaboration, treatment is fostered through integrated professional and community support, and the social determinants of health are considered in understanding the patient’s relationship to his/her presenting concerns. The Center for Substance Abuse Treatment (2019) explains that building relationships across the service system, provider networks, and the local community boosts trauma-informed care continuity when patients are involved in multiple services at one time. Table 2 depicts the stages of behavioral health integration.
Treatments such as cognitive behavioral therapy (CBT) and prolonged exposure therapy are proven effective in treating patients diagnosed with PTSD. Comparable to principles of the Biodyne Model, trauma-informed care allows patients to be fully engaged in their treatment process through interdisciplinary collaboration, treatment is fostered through integrated professional and community support, and the social determinants of health are considered in understanding the patient’s relationship to his/her presenting concerns. The Center for Substance Abuse Treatment (2019) explains that building relationships across the service system, provider networks, and the local community boosts trauma-informed care continuity when patients are involved in multiple services at one time. Table 2 depicts the stages of behavioral health integration.
Table 2: Stages of Behavioral Health Integration
|
Coordinated |
Co-located |
Integrated |
|
Behavioral health and other healthcare professionals practice separately within their respective disciplines. Details regarding shared patients are exchanged when necessary and there is limited collaboration. |
Behavioral health and medical providers practice in the same office. Co-location depicts where services are provided rather than a particular service. Therefore, patient care is often limited to each provider’s area of expertise. |
Behavioral health and medical providers collaborate and create patient treatment/care plans. There exist closely integrated, on-site efforts with a unified care plan. Additional on-site services like social services may also be available. |
Content adopted from Agency for Healthcare Research and Quality. (2011). Lexicon for behavioral health and primary care integration. Retrieved on December 1, 2013 from http://integrationacademy.ahrq.gov/lexicon
The goal of the Biodyne Model is to produce life change. In assessing the medical and mental health impacts of trauma throughout one’s developmental years, it is crucial to consider which techniques can be employed to support this goal. For instance, the Biodyne Model uses various treatment strategies such as relaxation, systematic desensitization, reinforcement schedules, homework assignments, cognitive restructuring, and role playing (Cummings et al, 2013). Additionally, preventative, or management efforts can be offered from professional to patient via psychoeducation, linkage to community health referrals, and health equity. Health equity can be achieved when everyone is afforded the same opportunities to be as healthy as possible. This may be accomplished by increasing provider awareness on health disparities, expanding healthcare coverage, improving existing coverage, and creating local efforts to not solely educate, but create opportunities for healthier standards of living (Mayne, 2023).
In addition, creating a clinical pathway which engages notions of the Biodyne Model, applies trauma-informed principles, utilizes a professional referral system, and links community support services considering the social determinants of health may establish an innovative standard of practice. Early psychoeducation efforts can be promoted through community engagement to encourage health and wellness, and further facilitate preventative strategies. Upon entering treatment, warm handoffs between medical doctors and behavioral create a foundational understanding of diagnosis and appropriate treatment considerations. Additionally, culturally sensitive, peer-led community and health care professional education is a necessary step in CVD prevention (Mehta et al., 2023).
 Conclusion
Conclusion
There is a proven link between a person’s medical health and mental health, and the prevalence of comorbid conditions is high among women. Understanding the physiology of trauma in conjunction with developing medical conditions is a concern worth continual research. In the meantime, the utilization of integrated healthcare treatment in managing these interconnected issues is significant to reducing cost, prevalence, and morbidity.
References
Administration for Children and Families. (n.d.). Trauma. Administration for Children and Families. https://www.acf.hhs.gov/trauma-toolkit/trauma-concept
Agency for Healthcare Research and Quality. (2011). Lexicon for behavioral health and primary care integration. Retrieved on December 1, 2013 from http://integrationacademy.ahrq.gov/lexicon
American Heart Association. (2017, May 31). What is Cardiovascular Disease? Www.heart.org; American Heart Association. https://www.heart.org/en/health-topics/consumer-healthcare/what-is-cardiovascular-disease
American Psychological Association. (2021). Trauma and Shock. American Psychological Association. https://www.apa.org/topics/trauma
American Thyroid Association. (2016). General Information/Press Room | American Thyroid Association. American Thyroid Association. https://www.thyroid.org/media-main/press-room/
CDC. (2023). Heart Disease Risk Factors. Centers for Disease Control and Prevention. https://www.cdc.gov/heartdisease/risk_factors.htm
Centers for Disease Control and Prevention. (2022, June 22). Preventing sexual violence. Centers for Disease Control and Prevention. https://www.cdc.gov/violenceprevention/sexualviolence/fastfact.html
Center for Substance Abuse Treatment . (2019). Trauma-Informed Care: A Sociocultural Perspective. Nih.gov; Substance Abuse and Mental Health Services Administration (US). https://www.ncbi.nlm.nih.gov/books/NBK207195/
Cherry, K. (2021). What Are the Signs of PTSD in Women? Verywell Mind. https://www.verywellmind.com/ptsd-in-women-signs-and-symptoms-5198684
Chu, B., Marwaha, K., Ayers, D., & Sanvictores, T. (2022, September 12). Physiology, Stress reaction. PubMed; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK541120/
Companies, S. (2023, May 3). Post-Traumatic Stress Disorder in Women: Signs & Symptoms. Capital Women’s Care. https://www.cwcare.net/post-traumatic-stress-disorder-in-women-signs-symptoms/
Cummings, N. A., & Cummings, J. L. (2013). Refocused psychotherapy as the first line intervention in behavioral health. Routledge.
Davis, L. L., Schein, J., Cloutier, M., Gagnon-Sanschagrin, P., Maitland, J., Urganus, A., Guerin, A., Lefebvre, P., & Houle, C. R. (2022). The Economic Burden of Posttraumatic Stress Disorder in the United States From a Societal Perspective. The Journal of Clinical Psychiatry, 83(3). https://doi.org/10.4088/jcp.21m14116
Federal Data | Youth.gov. (2019). Youth.gov. https://youth.gov/youth-topics/violence-prevention/federal-data
Galli, F., Lai, C., Gregorini, T., Ciacchella, C., & Carugo, S. (2021). Psychological Traumas and Cardiovascular Disease: A Case-Control Study. Healthcare, 9(7), 875. https://doi.org/10.3390/healthcare9070875
Gerber, M. R., & Gerber, E. B. (2019). An Introduction to Trauma and Health. Trauma-Informed Healthcare Approaches, 3–23. https://doi.org/10.1007/978-3-030-04342-1_1
Harper, C. R., Li, J., Sheats, K., Hertz, M. F., Merrill-Francis, M., Friar, N. W., Ashley, C. L., Shanklin, S., Barbero, C., Gaylor, E. M., & Hoots, B. E. (2023). Witnessing Community Violence, Gun Carrying, and Associations with Substance Use and Suicide Risk Among High School Students — Youth Risk Behavior Survey, United States, 2021. MMWR Supplements, 72(1), 22–28. https://doi.org/10.15585/mmwr.su7201a3
Mayne, S. (2023). Population Health Intervention: Thyroid Disease and Mental Health. Cummings Graduate Institute.
Mehta, L. S., Velarde, G. P., Lewey, J., Sharma, G., Bond, R. M., Navas-Acien, A., Fretts, A. M., Magwood, G. S., Yang, E., Blumenthal, R. S., Brown, R.-M., & Mieres, J. H. (2023). Cardiovascular Disease Risk Factors in Women: The Impact of Race and Ethnicity: A Scientific Statement From the American Heart Association. Circulation. https://doi.org/10.1161/cir.0000000000001139
National Children’s Alliance . (2023). National Child Abuse Statistics from NCA. National Children’s Alliance. https://www.nationalchildrensalliance.org/media-room/national-statistics-on-child-abuse/#:~:text=More%20than%20600%2C000%20children%20are
National Coalition Against Domestic Violence. (2021). National Statistics. NCADV. https://ncadv.org/statistics
Novotney, A. (2023). Women who experience trauma are twice as likely as men to develop PTSD. Here’s why. Apa.org. https://www.apa.org/topics/women-girls/women-trauma
Ohrnberger, J., Fichera, E., & Sutton, M. (2017). The relationship between physical and mental health: A mediation analysis. Social Science & Medicine, 195(195), 42–49. https://doi.org/10.1016/j.socscimed.2017.11.008
Olff, M. (2017). Sex and gender differences in post-traumatic stress disorder: an update. European Journal of Psychotraumatology, 8(sup4), 1351204. https://doi.org/10.1080/20008198.2017.1351204
Ramanuj, Parashar & Ferenchik, Erin & Docherty, Mary & Spaeth-Rublee, Brigitta & Pincus, Harold. (2019). Evolving Models of Integrated Behavioral Health and Primary Care. Current Psychiatry Reports. 21. 10.1007/s11920-019-0985-4.
Sheng, J. A., Bales, N. J., Myers, S. A., Bautista, A. I., Roueinfar, M., Hale, T. M., & Handa, R. J. (2021). The Hypothalamic-Pituitary-Adrenal Axis: Development, Programming Actions of Hormones, and Maternal-Fetal Interactions. Frontiers in Behavioral Neuroscience, 14(601939). https://doi.org/10.3389/fnbeh.2020.601939
Substance Abuse and Mental Health Services Administration. SAMHSA’s working definition of trauma and principles and guidance for a trauma-informed approach. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2012.